
Hysteroplasties: do uterine malformations always need to be corrected?
Surgical correction techniques performed on uterine malformations are known as hysteroplasties and metroplasties.
The most recent classification published by the European Society of Human Reproduction and Embryology (ESHRE) states that between 4 and 7% of the general population suffers from congenital malformations of the female genital tract. Even though malformations of this kind are benign, depending on what type of malformation the patient has, it can be linked to other health and reproduction issues.
So, when a patient is diagnosed as having a malformation of the female genital tract, is surgical intervention always the way forward?
The data provided in scientific evidence clearly indicates that patients with malformations of the uterus are at a greater risk of experiencing obstetric complications such as spontaneous pregnancy losses, premature childbirth, intrauterine growth restriction, postpartum metrorrhagia and bleeding during pregnancy, incompetent cervix, malpresentations, pre-eclampsia and childbirth by Caesarean section.
Surgical procedures to correct malformations of the uterus have been described since the 19th century and can provide a solution for patients with complications of this kind.
However, hysteroplasties should only be performed when a malformation in the uterus is associated with recurrent premature births, unexplained infertility and, exceptionally, in cases of severe dysmenorrhea.
Several invasive and non-invasive surgical procedures aimed at correcting these abnormalities have been proposed. However, some of them, such as surgical correction of a bicornuate uterus, do seem to be more harmful than others and, as such, they are not performed as a matter of routine. Nonetheless, surgical removal of the uterine wall is linked to a decreased risk of pregnancy loss and should be offered as a solution to women who have experienced recurrent losses.
Hysteroplasties must be performed during the early follicular phase (between days 6 and 10) or on patients who have undergone endometrium preparation over the month leading up to the intervention. This generally consists of taking contraception pills and the aim is to aid the planning process, ensure that the patient is not pregnant and perform the operation on a hypertrophic endometrium.
The type of hysteroplasty that is performed depends on the type of malformation.
ESHRE has described 5 main groups classifying female genital tract malformations in patients with a dysmorphic uterus, septate uterus, bicorporeal uterus, hemi-uterus or aplastic uterus.
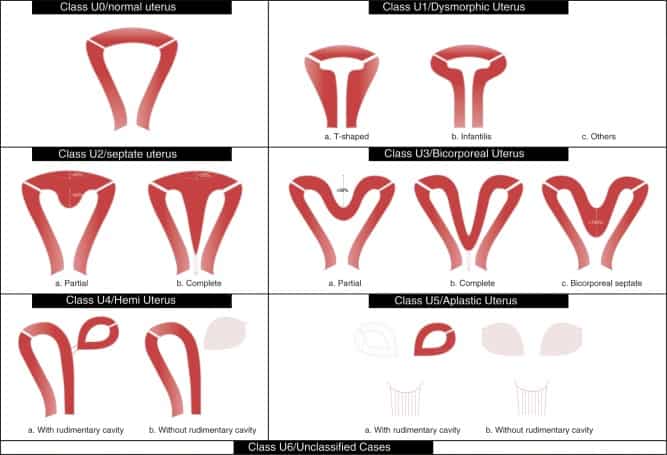
- T-shaped uterus (hypoplasia of the uterus). This is a rare malformation and has mainly been described in patients who experienced intrauterine exposure to diethylstilbestrol in France up until 1977. This malformation falls into ESHRE category type U1. We must differentiate between harmonious hypoplasias of the uterus, or uterus infantilis, (liked to hypoestrogenism and frequently associated with primary amenorrhea) and T-shaped hypoplasias, since the harmonious type should not be considered for surgery under any circumstances.
The applicable surgical intervention in this case would be a hysteroplasty enlargement using hysteroscopy techniques. The existing lack of knowledge means there are currently no clear indications about when this intervention should be performed. It should not be performed systematically as a first option when a patient does not show signs of infertility or issues during pregnancy. However, this kind of intervention would be justified if the patient has experienced recurrent pregnancy losses or has failed to get pregnant following recurrent attempts at assisted reproduction.
- Septate uterus. This malformation is the most common of all (present in 1% of the female population) and it is classed by ESHRE as type U2.
A septate uterus malformation can be complete with a maximum vaginal and cervical wall, partial septate, or a simple fundic spur. The walls are never associated with malformations in the urinary apparatus.
Surgery is advised when the patient has a background of recurrent early or late pregnancy losses and premature childbirth. It is currently very difficult to provide patients who have a septate issue with a clear answer as to whether or not they should wait for an obstetric issue to arise before opting for surgery. The procedure involves using hysteroscopy techniques to perform a hysteroplasty through a section of the uterine wall and not a resection. The aim is to preserve as much of the endometrium as possible.
- Surgical procedures cannot be performed on a bicornuate or unicornuate uterus. Bicornuate uteri are five times less common than septate uteri. The prognosis in spontaneous obstetrics and in assisted reproduction are very similar to those for unicornuate uteri, but there is no effective available surgical treatment. It has been reported that there are no obstetric benefits to hysteroplasties with the traditional Strassman’s method and, as such, they should not be performed.
Bibliography
- Congenital Uterine Malformations (CONUTA) common ESHRE/ESGE Working Group. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Human Reproduction 2013; 28 (8): 2032–2044
- Pourcelot AG, Fernandez H. Tratamiento quirúrgico de las malformaciones uterovaginales. EMC – Ginecología-Obstetricia 2019; 55 (1): 1-10 [Artículo E – 41-675]
- Parisot-Liancea L, Capmasabc P, Levaillanta JM, Fernandez H. Histeroplastia de aumento. EMC – Ginecología-Obstetricia 2021; 57 (2): 1-8
- Narvión Casorrán C, González Díaz I, Peña y Lillo Rodríguez A, Albi Martín B, Díaz Toledo Núñez de Arenas B, Escribano Tórtola JJ. Gestación satisfactoria tras metroplastia de Strassman en mujer con útero bicorne. Prog Obstet Ginecol. 2017; 60 (4): 368-372
- Savey L, Le Tohic A. Malformaciones uterinas. Ginecología. Elsevier SAS, París, 2003. E – 123·A·10
Dr Blanca Bayoumy, gyneacologist at Instituto Bernabeu
