Sperm retrieval techniques: Biopsy and testicular puncture (TESA and MESA)
Through these techniques, sperm can be retrieved in cases -such as azoospermia- where they are not found in the ejaculate, hence allowing fertilization with the patient’s own gametes
In modern medicine, sperm can be collected for the purposes of assisted reproduction in many different ways. The chances have been increased, treatment aggressiveness has been reduced and sample quality has been improved. From vasectomised, males to cases of sperm pathway obstruction or cystic fibrosis. Satisfactory sperm can be collected with a simple puncture of the testicles under regional anaesthesia. Biopsy in its different modalities is also advised in certain cases.
Working with our Reproductive Biology Laboratory in real time is essential, as well as their preparation and dedication to the reproductive process, which enhances the results considerably.
What does testicular biopsy involve?Testicular biopsy is a surgical operation through which only the best sperm are collected. It involves slitting open 2-3 centimetres of the testicle skin to collect testicular tissue and, therefore, sperm. Testicular material is then fractioned; one part is meant for reproduction techniques and the other for testing. Sometimes several samples are taken (two or three from different parts of each testicle) in special cases. It is generally performed under sedation, although it can also be done under regional anaesthesia, depending on the patient’s tolerance. There are different types of biopsy and different techniques (loupes, TESE, MicroTESE). |
Once the testicular tissue has been collected, we can pursue two goals:
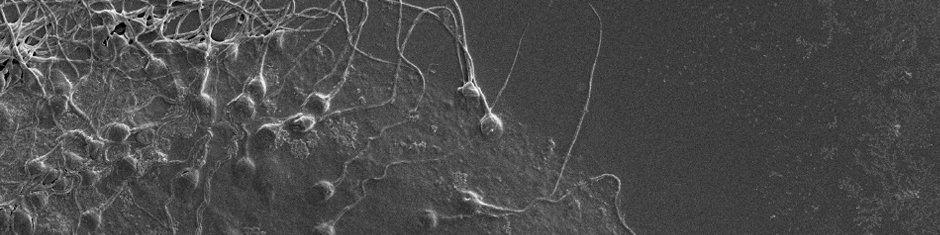
1. Analyzing the testicular tissue and its capacity to produce sperm, and find out the point in spermatogenesis where production is interrupted. Analyses of cell division are carried out, focusing on the structure, the composition and the order of chromosomes throughout the different stages of sperm formation. This helps to rule out male causes for recurrent miscarriages. This type of biopsy is generally practiced to find the cause of male infertility whenever a spermiogram shows abnormal sperm and the cause has not been found with other tests. In this way, it is indicated for cases of azoospermia, oligozoospermia and severe alterations in sperm quality where there may be a high risk of sperm chromosomal anomalies.
2. Retrieving live sperm in order to inject one into each of the couple’s eggs, having previously retrieved the eggs by ovarian stimulation and puncture. This is done in cases where the seminal ducts are obstructed, possibly as a result of a number of causes, both congenital and acquired. Among the congenital causes, the absence of vasa deferentia is the most frequent. It is commonly associated with a disease called cystic fibrosis. Other causes of obstruction are of an infectious, traumatic and surgical nature (such as they occur after a vasectomy). Yet, the causes of obstructions are often not satisfactorily found.
Testicular biopsies for sperm retrieval are usually not performed for diagnosis prior to In Vitro Fertilization treatments with ICSI. They are performed on the same day as egg retrieval. Otherwise, the retrieved sperm would have to be frozen and subsequently thawed for their use. Sperm freezing resulting from a previous biopsy, may compromise the quality and survival of some of the sperm.
Testicular puncture or testicular biopsy: Which one is better?
The purpose of both is retrieving the most appropriate testicular material (sperm) for a successful assisted reproduction treatment that is as harmless as possible. It is the biologist’s duty to establish whether the sample is just appropriate or the best sample possible. The biologist will be working on the sample and will assess it in real time from the moment of retrieval. Accordingly, s/he will request more or less material from the urologist as needs be. Similarly, the urologist’s duty is to provide the best material (sperm) while minimizing the possible damage done to the testicles. To achieve this, we have a team of specialist urologists at Instituto Bernabeu, in addition to our reproductive biology team.
It should be pointed out that in many cases the material retrieved by puncture can be as good as the material retrieved with a testicular biopsy. However, as far as biopsies are concerned, the pain suffered, the damage done to the testicles, the risks and the recovery process may be different. One must also keep in mind that these procedures may have to be performed more than once.
The selection of one sperm retrieval technique or the other is based on a number of conditions revealing which one is more appropriate. In patients with testicular abnormalities, such as simultaneous hydrocele, loss of testicular consistency, previous testicular surgeries, hormonal alterations and need of a histological study of the testicles, a testicular biopsy is more adequate because more material is retrieved, it is possible to prove the absence of sperm and a histological study of the testicles can be carried out. The resulting information cannot be obtained by puncture.
The advantages of puncture in those cases where it is performed is that the necessary material can be retrieved and no further damage is done to the testicles. It is also less expensive. The quality of the material should not vary according to the technique whereby it is retrieved but to what is retrieved from the patient’s testicles. If the material retrieved by puncture turned out to be insufficient, a biopsy could be performed as per the biologist’s instructions.
As we have seen, neither technique is better than the other. Only a careful selection will result in the best material and diagnosis and the least damage possible.