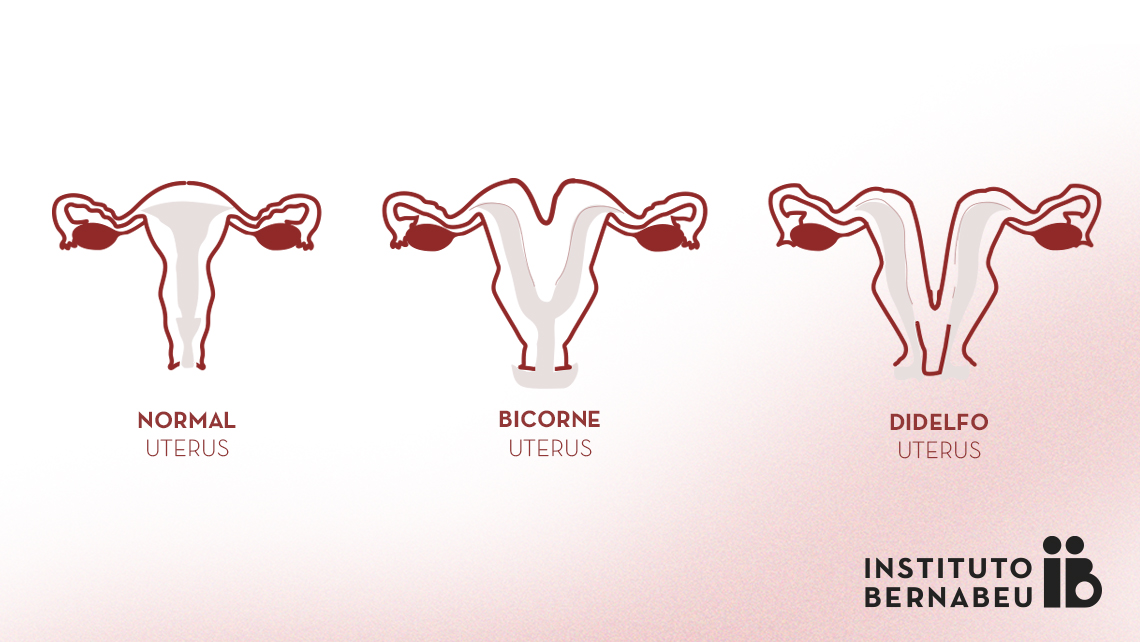
Bicornuate uterus, double uterus or uterus didelphys: what is it? How can it affect fertility and pregnancy?
Congenital abnormalities of the uterus, also known as Müllerian duct anomalies, are classed according to the defect generated during development of the organ in the pre-embryo stage. That is, the uterus is formed through development of two lateral tubes, known as the paramesonephric ducts, that fuse together. Reabsorption of the septum that remains is required in order to leave just a single cavity that becomes the endometrial cavity. Müllerian ducts form the uterus, the Fallopian tubes and the top third of the vagina. Therefore, uterine malformations do not necessarily have to be deformations in the ovaries or of the lower two-thirds of the vagina. However, it is linked to formation of the nephro-urological system and, as such, when there is a uterine malformation, the patient must be checked for kidneys and ureters.
Prevalence
Bicornuate uteri are present in 0.4% of the general population, in 1.1% of women who are infertile, in 2.1% of women who have had a pregnancy loss and in 4.7% of women who are infertile and have had a pregnancy loss. Most patients with a bicornuate uterus do not develop any symptoms during adolescence. Some women attend a clinic to deal with menorrhagia (heavy menstrual bleeding) or dysmenorrhea (intense menstrual pain) since they suffer from endometriosis, which is closely linked to the condition. However, most patients never have any symptoms.
Diagnosis
Further to progress in our understanding of each type of malformation and its consequences, there have been a number of changes to how they have been categorised. Non-invasive diagnosis can be performed using a magnetic resonance scan or three-dimensional ultrasound. These methods can be used to view the external contour of the uterus and internal contour of the endometrial cavity. While hysterosalpingographies have frequently been used for this purpose, malformations that affect the external contour of the uterus cannot be diagnosed with this method. Nonetheless, a hysteroscopy and laparoscopy can be performed simultaneously in order to achieve a confirmed diagnosis, even if this method is invasive. Nowadays, it is now used only in very specific cases.
A so-called double uterus or uterus didelphys is currently known as a complete bicornuate uterus based on the most recent categorisation developed by the European Society of Human Reproduction and Embryology (ESHRE) in 2013. It is produced by a defect in the fusion of the paramesonephric ducts. According to the ESHRE nomenclature, it is a Class U2b and anomalies in the cervix can also be present. There may be a double cervix or double vagina and a longitudinal septum separating them in two.
Diagnosis must be performed by viewing a dip in the external uterine contour that completely divides the uterine as far as the cervix.
Treatment
Treatment for bicornuate uteri is not generally required . However, there is surgical treatment known as the Strassman’s metroplasty, which entails joining the two uteri externally and making an incision in the wall to join the two endometrial cavities. Indications for this surgery do not currently exist since no well-designed meta-analyses or studies have been able to demonstrate that it improves the patient’s clinical condition compared with refraining from having any treatment.
During pregnancy, patients with a bicornuate uterus are at a greater risk of pregnancy loss in the first and second terms, premature birth, a low weight at birth and an abnormal position of the foetus. Therefore, strict controls during pregnancy, particularly of the length of the cervical canal, are required in order to avoid the birth of a premature child.
Dra. Belen Moliner, gyneacologist at Instituto Bernabeu
