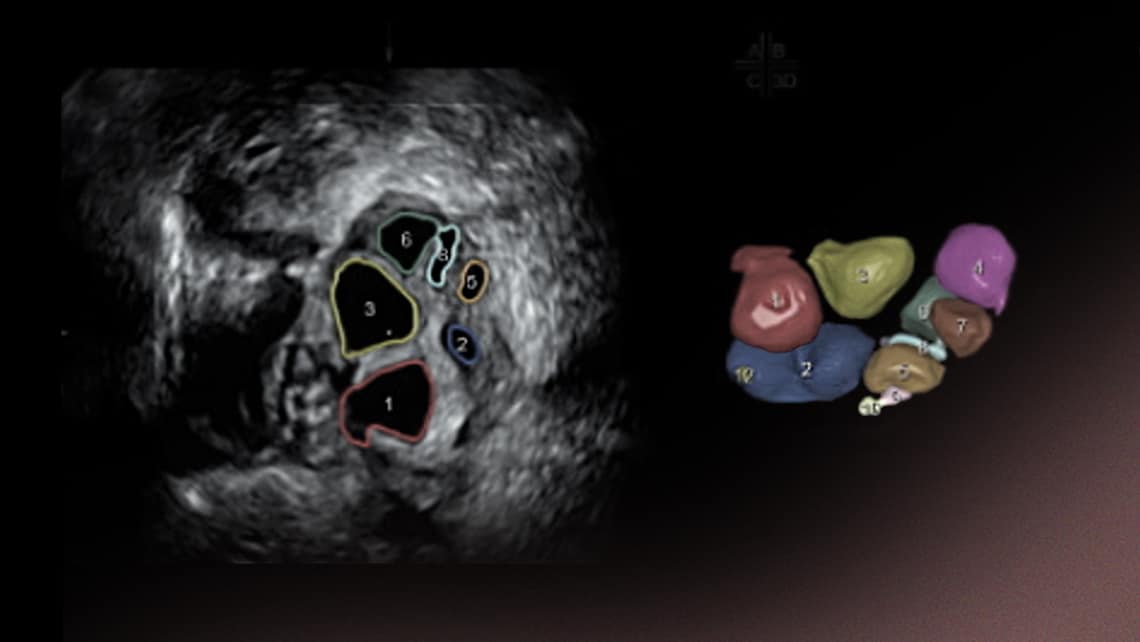
Basal ultrasound scan: antral follicle count to determine ovarian reserve
The antral follicle count (AFR) is one of the first tests to be performed on a woman undergoing infertility testing. It’s a transvaginal ultrasound in which the number of follicles – cystic structures that form the eggs during their maturation process – a woman has in a menstrual cycle is evaluated, which in turn is related to ovarian reserve.
Índice
- 1 What is a basal ultrasound scan?
- 2 What are the antral follicles?
- 3 At what time of the cycle should basal ultrasound be performed to evaluate antral follicles?
- 4 What is anormal number of antral follicles?
- 5 Can antral follicle values vary from month to month?
- 6 What is the purpose of follicles ultrasound at basal time and in which cases is it indicated?
- 7 Antral follicle count as a predictor of ovarian reserve
- 8 What other diagnostic tests can assess ovarian reserve?
What is a basal ultrasound scan?
Basal ultrasound is the uterus and ovaries evaluation at the beginning of the menstrual cycle, generally in the first 5 days of the menstrual cycle, by performing a transvaginal ultrasound.
What are the antral follicles?
Antral follicles are cystic, i.e. liquid-containing, structures that form oocytes in the early stages of their maturation in response to the secretion of follicle-stimulating hormone (FSH).
In a normal menstrual cycle, a variable number of oocytes begin to develop and can be seen as small cysts of between 2 and 10 millimetres on gynaecological ultrasound. Then, as the cycle progresses and generally from the 8th day onwards, one of these follicles will dominate over the rest, increase in size to 18-27 millimetres and produce the oestradiol hormone, which in turn causes the endometrium in the uterus to grow in order to accommodate the pregnancy. Finally, the increase in oestradiol stimulates the secretion of luteinising hormone (LH), which will trigger the rupture of the dominant follicle leading to ovulation, where the mature egg can be captured by the fallopian tubes and fertilised by a sperm. The empty follicle will collapse to form the corpus luteum, which produces progesterone to maintain a possible pregnancy, and if this does not occur it will end up being reabsorbed and trigger the period as the hormonal levels fall.
Antral follicles that have not matured will also be reabsorbed, disappearing through a process called follicular atresia.
At what time of the cycle should basal ultrasound be performed to evaluate antral follicles?
In general, the best time to assess them is between the 2nd and 4th day of menstrual bleeding; although some studies have shown that they can also be assessed in the second half of the cycle without losing predictive power for the assessment of ovarian reserve.
What is anormal number of antral follicles?
As with ovarian reserve, the number of antral follicles correlates with age, and what we consider normal depends on age. In a woman under 35 we should see at least 10 antral follicles between the two ovaries, and below 5-7 is considered low ovarian reserve.
Can antral follicle values vary from month to month?
The antral follicle count as a test of ovarian reserve has some limitations, with variations from cycle to cycle, although generally small, and for this reason it’s often combined with the anti-mullerian hormone (AMH) value which does not experience these fluctuations. In addition, it’s an operator-dependent technique, so it will require a trained gynaecologist and a high-resolution ultrasound scanner.
What is the purpose of follicles ultrasound at basal time and in which cases is it indicated?
Basal ultrasound in the first days of the cycle has a prognostic value in infertility. It helps us predict the ovarian response in patients who must undergo ovarian stimulation and subsequent in vitro fertilisation (IVF), and thus to estimate the possibility of pregnancy in this treatment. Depending on the ovarian reserve, as well as other characteristics of the patient (age, body mass index, response to previous cycles, and sometimes even genetic profile), we will plan the most appropriate treatment for her. In addition, at the start of ovarian stimulation, it will allow us to check the situation of ovarian rest, i.e. that there’s no residual cyst in the ovaries that could interfere with the medication.
On the other hand, the antral follicle count can be done in non-infertile women under 40 years of age, allowing individualised counselling of their reproductive options, as if it is low, it indicates an increased risk of menopause in 5 years.
Antral follicle count as a predictor of ovarian reserve
Antral follicle count is considered one of the best tests of ovarian reserve, being non-invasive and relatively simple to perform.
We call ovarian reserve to the available eggs at a given time in a woman’s ovary, which can vary over time since eggs are produced in foetal life and do not regenerate again after birth, so that they are progressively consumed until menopause.
It is important to clarify that ovarian reserve is not related to the possibilities of natural pregnancy, for which only one egg needs to mature per month as occurs in the normal cycle; but it’s associated with the possibilities of pregnancy in IVF, since in the process of ovarian stimulation we take advantage of this «excess» recruitment the ovary makes every month to mature several eggs at the same time and thus multiply the possibilities of pregnancy. This way, ovarian stimulation doesn’t damage the ovarian reserve either, as it uses the oocytes that would be destined to be lost through atresia in that cycle.
Finally, as mentioned above, the ovarian reserve will also indicate the risk of menopause in the next 5 years.
What other diagnostic tests can assess ovarian reserve?
The anti-mullerian hormone (AMH) produced in the ovary and valued by means of a blood test, together with the antral follicle count, is currently considered the best test for estimating ovarian reserve. Both are quantitative tests, they tell us about the number of eggs, but not their quality, for the determination of which there’s no current test available and which again is closely related to age.
Other tests, such as basal FSH in the first 5 days of menstruation, can be used to assess ovarian reserve. As explained above, FSH stimulates the follicles containing the eggs to mature. When the ovary is in a state of exhaustion, FSH increases in an attempt to compensate, which can be demonstrated analytically even several years before the menopause occurs. Likewise, a decrease in ovarian blood flow on ultrasound, and the continued shortening of cycles, may indicate a compromised ovarian reserve.
Dr Esperanza de la Torre, gynecologist at Instituto Bernabeu
IT MAY ALSO BE OF INTEREST TO YOU:
