Do I suffer from low ovarian response? how should I treat it?
We refer to low response when the number of eggs obtained in a patient during an IVF cycle is lower than expected. A patient is defined as a low responder when 3 or less eggs are collected or when the ovarian reserve markers (antimüllerian hormone and antral follicle count) are low.
As the number of eggs obtained in a treatment is one of the most important prognostic factors in the treatment’s success, in these patients the chances of pregnancy may be compromised. For this reason, a global evaluation of the case by a multidisciplinary team is essential. Thus, gynaecologists, embryologists, and specialists in molecular biology and genetics work to design a strategy that optimises the chances of achieving the birth of a healthy newborn.

Identified the genes involved in ovarian reserve

Personalized treatment plan

Pharmacogenetics: higher response medication

Higher number of eggs
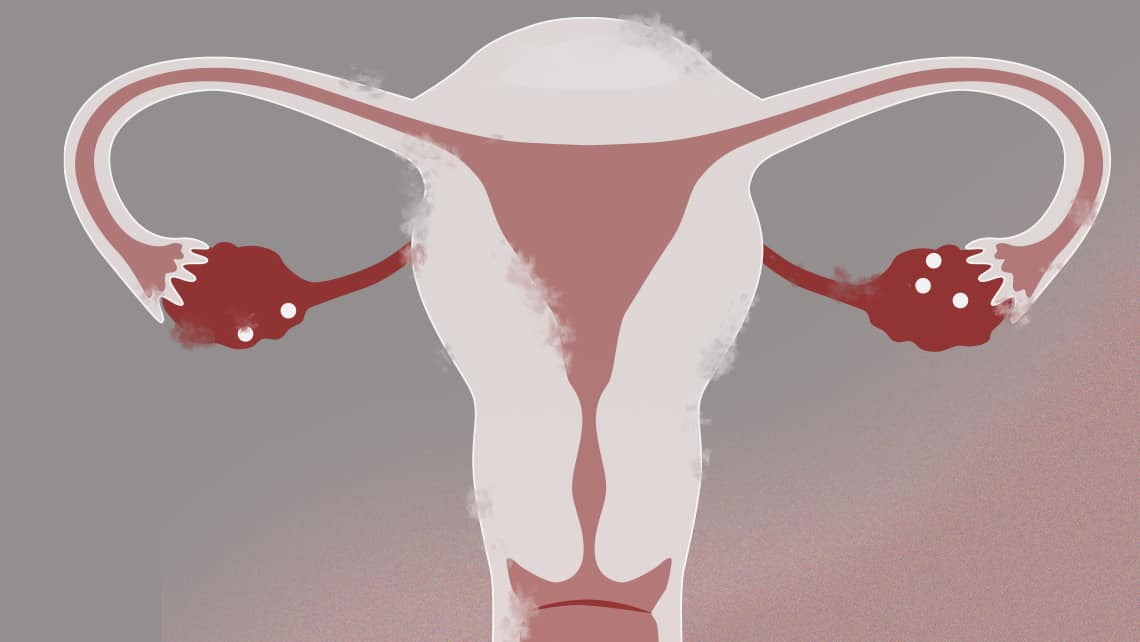
Age is the most important factor, but there’re also pathologies that cause a low response and can threaten the woman or her future offspring’s health. For this reason is essential to carry out diagnostic tests to rule out diseases such as endometriosis, immunological conditions or genetic alterations.
The Genetics Unit at Instituto Bernabeu studies the genetic causes of low ovarian response, such as karyotype abnormalities or X-Fragile Syndrome, preventing the birth of a child with serious genetic diseases. On the other hand, different genes involved in family cases of early ovarian failure or early menopause have recently been evaluated, which will make it possible to identify cases of genetic origin and locate those family members at risk, with the possibility of planning their reproductive life or preserving eggs for the future.
Low ovarian response treatment will be aimed at increasing the number of oocytes obtained. In our opinion, the strategy should start with conventional stimulation protocols, being an individualised approach of main importance. Thus, some patients will benefit from the use of adjuvant drugs or mild protocols to improve response. Once again, the role of genetics will be important, as after years of research, Instituto Bernabeu has identified the genes involved in ovarian response. For this, we are currently using the IBGENFIV genetic test, which allows the medical team to determine the most appropriate medication for the patient’s genetic profile.

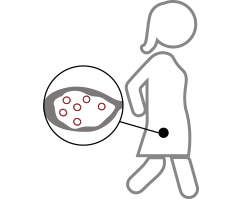
A strategy that has significantly improved the prognosis of these patients has been the accumulation of eggs from several stimulation cycles. This allows us to carry out the in vitro fertilisation cycle with a number of eggs similar to that of the normo-responder patient. A key factor in this has been the appearance of the oocytes vitrification technique, which allows eggs to be preserved in the laboratory with a very high survival rate. Accumulation has the advantage of being able to have a greater number of eggs in a shorter period of time, an important factor in many cases due to age or underlying pathology. On the other hand, costs will be reduced because the fertilisation process will only be carried out once.
The Low Reserve Unit has developed different stimulation strategies for oocyte accumulation. We now know that we can perform stimulation at different times of the menstrual cycle. Thus, we can perform a conventional stimulation, at the beginning of the menstrual cycle, but also after ovulation, which is called luteal phase stimulation. We can even perform two stimulations within the same cycle, the double ovarian stimulation. Both strategies have improved the response in many patients.
Recently, “ovarian activation” treatments have been implemented and its results, still experimental, are promising. Thus, some patients with low ovarian response could benefit from the administration of platelet-rich plasma into the ovary, which can activate eggs that remain inactive or “dormant” in the ovary of these patients. Also, ovarian cortex fragmentation and autotransplantation (OFFA) aims at ovarian activation in patients with early ovarian failure or early menopause.
