
How Fertility Has Declined: Causes, Impact, and Prevention
Infertility is not an isolated phenomenon or a specific problem affecting only a few couples; it is a growing public health challenge. According to the World Health Organization (WHO), it now affects 17.5% of the global reproductive-age population. In Spain, figures range between 10% and 15%, with a rising trend that shows no signs of slowing down in the coming years.
What is concerning is that these percentages reflect profound changes in our reproductive health, influenced by biological, social, environmental, and healthcare factors. Below, we analyze the main factors responsible for this decline in fertility in a clear and understandable way.
Índice
Delaying Motherhood: A Trend with a Direct Impact on Women
One of the factors that most clearly explains this decrease in fertility is the delay of motherhood. Today, many women decide to become mothers after age 35, an age at which fertility decreases significantly.
This occurs for strictly biological reasons:
- The quantity of eggs progressively decreases (ovarian reserve).
- Oocyte quality is compromised by genetic aging.
- The risk of chromosomal alterations and reproductive complications increases.
Added to this are relatively common pathologies such as Polycystic Ovary Syndrome (PCOS), endometriosis, premature low ovarian reserve, or certain thyroid alterations, which can directly affect reproductive capacity.
The result is that, after age 35, achieving a natural pregnancy can be significantly more difficult—not due to social reasons, but primarily because of a biological limit.
Male Fertility Is also on the decline
For a long time, male fertility was considered stable. However, scientific evidence from recent decades points in the opposite direction.
Sperm concentration has decreased by approximately 50% since 1973, and this is not an isolated finding: various international studies and reviews confirm a global downward trend. So much so that the WHO has had to update its semen quality criteria because values previously considered “normal” no longer represented the current population.
Among the possible causes, we find:
- Genetic or hormonal alterations.
- Testicular problems.
- Environmental factors and lifestyle habits (with varying degrees of scientific strength).
The combination of these elements can result in lower sperm concentration, poorer motility, higher DNA fragmentation, and real difficulties in achieving pregnancy.
STIs: A Silent Problem Affecting Fertility Without Symptoms
Another key factor that often goes unnoticed is Sexually Transmitted Infections (STIs). More than 30 different types can affect humans, and many of them do not produce symptoms, which facilitates their transmission and hinders detection.
Among those caused by bacteria, viruses, and fungi, we find:
- Chlamydia
- Gonorrhea
- Syphilis
- HPV
- Hepatitis
- Herpes
The most worrying part is that, if not diagnosed in time, they can compromise both female and male fertility.
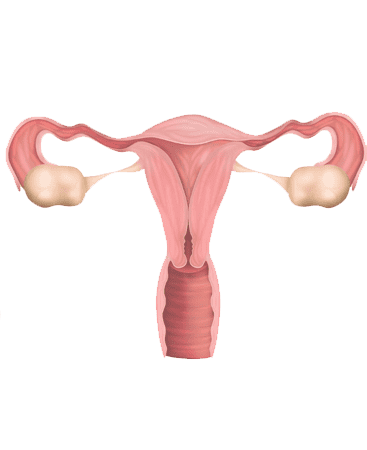
How do they affect women?
Untreated STIs can cause:
- Inflammation and blockage of the Fallopian tubes.
- Pelvic Inflammatory Disease (PID).
- Scarring that makes it difficult for the egg and sperm to meet.
- Increased risk of ectopic pregnancy and miscarriage.
In some cases, the consequences can be permanent.
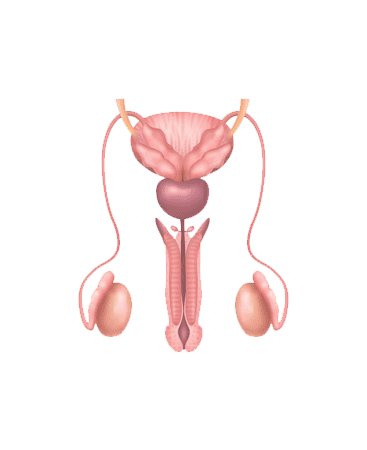
And how do they affect men?
In men, infections such as HPV, chlamydia, and gonorrhea can cause:
- Epididymitis (inflammation of the epididymis).
- Reduction in sperm count.
- Decrease in motility.
- Increased sperm DNA fragmentation.
This translates into a lower fertilizing capacity of the semen and, occasionally, the need to resort to assisted reproduction treatments.
The Specific Case of Chlamydia and Gonorrhea: Common, Silent, and Harmful
Chlamydia and gonorrhea are two of the most common STIs. Their main problem is that up to 70% of cases can be asymptomatic, allowing the infection to progress without the person knowing.
In women:
If undiagnosed and untreated, they can ascend from the vagina to the uterus, tubes, and ovaries, causing pelvic inflammatory disease. This can leave consequences such as:
- Tubal obstructions.
- High risk of ectopic pregnancy.
- Complications during pregnancy and childbirth.
- Transmission to the newborn, leading to serious infections in the baby.
In men:
In men, these infections:
- Inflame the epididymis.
- Damage the structure and function of the sperm.
- Reduce motility.
- Increase DNA fragmentation.
In the case of gonorrhea, the emergence of antibiotic-resistant strains adds an additional risk.
The Impact of Environmental Toxins and Endocrine Disruptors on Fertility
In addition to factors like age, infections, or semen quality, there is a less visible but increasingly relevant component in reproductive health: exposure to environmental toxins and Endocrine Disrupting Chemicals (EDCs). These compounds—present in air, water, plastics, pesticides, cosmetics, or industrial products—can interfere with the hormonal system and affect both female and male fertility.
Environmental toxins cover a wide range of chemical substances present in our surroundings. Among the best-known agents that can influence fertility are:
- Aromatic and halogenated hydrocarbons (benzenes, toluenes, phthalates).
- Organochlorine compounds (many pesticides).
- Heavy metals such as lead or cadmium.
- Substances found in plastics, cleaning products, or cosmetics.
Endocrine disruptors are compounds that alter the hormonal system by mimicking, blocking, or modifying natural hormone signaling. Since reproduction depends on a very delicate hormonal balance, even low-level interference can have significant effects on fertility.
How they affect female fertility
EDCs can alter key hormonal processes in women. Scientific evidence indicates that these toxins can:
- Interfere with egg maturation and quality.
- Alter ovarian function and ovulation.
- Contribute to disorders such as PCOS or uterine dysfunctions.
- Decrease the success rate of assisted reproduction treatments.
Furthermore, recent studies have detected persistent chemical substances even in the follicular fluid of the ovary, suggesting continuous exposure of the eggs to these agents.
How they affect male fertility
In men, environmental toxins and EDCs can also have adverse effects on sperm production and quality:
- Decrease in sperm concentration.
- Reduction in sperm motility and morphology.
- Increase in sperm DNA fragmentation.
- Alteration of the hormonal production necessary for the reproductive process.
Pollutants such as phthalates and bisphenols have been repeatedly highlighted in studies for their negative impact on testicular function and seminal health.
Factors Modulating the Risk of Toxins in Our Environment
The impact of toxins depends on several combined factors:
- Dose and duration of exposure: Chronic exposure, even at low levels, can have cumulative effects.
- Life stage during exposure: Critical periods such as fetal development, adolescence, or the preconception period are especially vulnerable.
- Combination of multiple chemicals: In real life, exposure occurs simultaneously to various substances, with possible synergistic effects.
What Can We Do? Practical Advice
Although it is not possible to completely eliminate exposure to all environmental toxins, the impact can be minimized by adopting simple measures:
- Choose products with fewer chemical ingredients (cosmetics, packaging, kitchen utensils).
- Avoid plastics, especially those with phthalates or bisphenol, when hot or in contact with food.
- Reduce exposure to pesticides by choosing organically produced food whenever possible.
- Ventilate indoor spaces and improve household air quality.
- Maintain a natural diet and healthy lifestyle habits (avoid tobacco and recreational drugs, moderate alcohol consumption).
