Types of endometrial receptivity test. Pros and cons
Embryo implantation in the endometrium is a key process in achieving pregnancy.
It takes place during a very short and specific period of time of the menstrual cycle in which the endometrium expresses specific molecules necessary for the embryo to nest.
Embryo implantation failure is a phenomenon widely studied in reproductive medicine and especially at Instituto Bernabeu, where we develop different R & D & I programs.
Traditional morphological markers to determine when an endometrium is receptive or not are not totally reliable and it’s necessary to use genomic molecular tools to help us in clinical practice.
Índice
What is the endometrial receptivity?
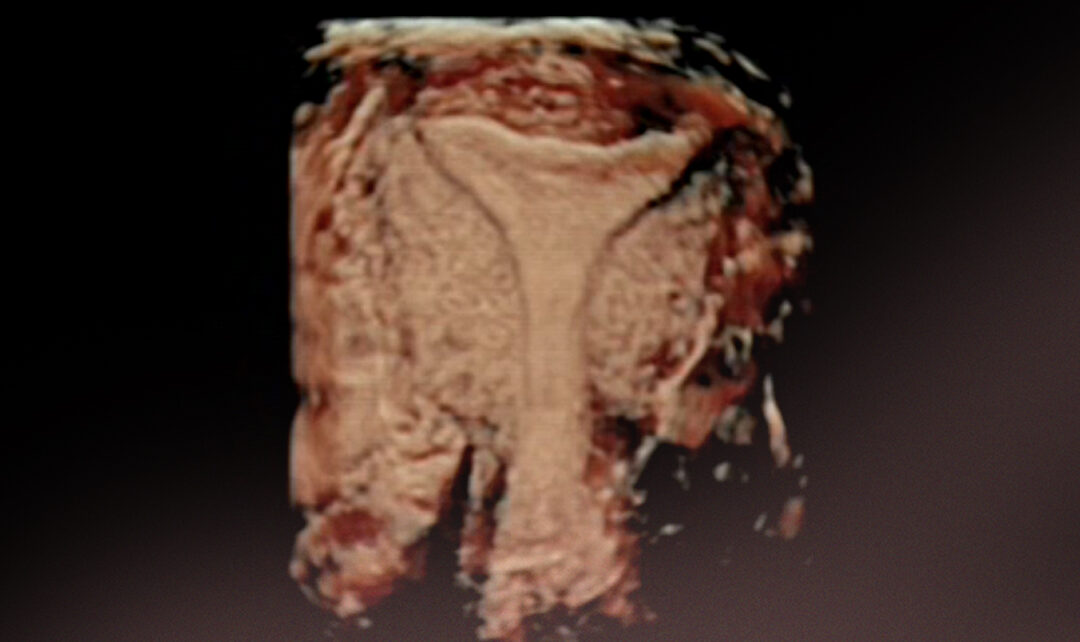
The endometrium is the tissue that lines the uterine cavity. For implantation to take place, the endometrium must be ready to “accept and host” the embryo.
This endometrium state is called endometrial receptivity and it’s observed to occur only at a certain time, around days 20-21 of the menstrual cycle, constituting the implantation window.
The endometrial receptivity state has a very specific gene activity profile, it has been studied that there are certain genes, called receptivity markers, that are expressed only during the implantation window.
It is also known that women with recurrent miscarriages or implantation failures have an altered expression of these endometrial receptivity markers during the embryo implantation window.
What kind of tools we have to study endometrial receptivity?
Histological analysis of endometrial biopsy
Throughout history, endometrial receptivity has been a widely studied phenomenon, Noyes in the 50s already established different patterns in terms of the cellular structure of the endometrium throughout the menstrual cycle.
Although the preferred technique to study the structure of the endometrium is endometrial biopsy, this also presents drawbacks because it is an invasive technique.
Ultrasound techniques
Endometrial visualization by ultrasound has traditionally been performed. There are several parameters to take into account to determine endometrial receptivity:
- Endometrial thickness
- Ultrasound pattern
- Endometrial volume
- Uterine contractility
However, these ultrasound techniques are not entirely accurate and we usually continue to encounter cases of implantation failures.
Endometrial genetics tests
These tests are trying to determine with greater accuracy the specific moment in which the endometrium is ready for the implantation of an embryo. They are based on 2 different concepts:
- transcriptomics or in
- microRNA expression
Endometrial receptivity test based on the transcriptome
It is widely known that each cell’s genetic information is found in its DNA chain, however, in order to use that information, cells need to read it and translate it into RNA.
The set of these RNA reads constitutes the TRANSCRIPTOME.
Through the study of the transcriptome, we can accurately know which genes are active or inactive in a certain cell or tissue at a specific time.
The ERA (Endometrial Receptivity Array) test uses this transcriptomic technology. More information
After several years using it, different investigations have emerged explaining that its use in general population is not always justified for different reasons (1 *) and (2 *).
Endometrial receptivity test based on microRNA expression
MicroRNAs are very small RNA molecules that can regulate gene expression and are highly involved in the embryo implantation process.
Recent studies reveal that miRNAs not only act inside cells, but can also be released into the extracellular environment. This fact could provide a new advance over implantation studies as they can serve as non-invasive biomarkers for the evaluation of endometrial receptivity.
The MIRA test is based on the study of these microRNAs
For or against endometrial genetics tests for endometrial receptivity?
However, these tests have great limitations. One of the most important is that a panel of genes which allows us to define exactly when the implantation window occurs has not yet been found.
Currently, there are several publications that question the real efficacy of these tests, and although the use of these technologies in the identification of endometrial receptivity is postulated as a great technological advance, further research is still necessary.
At Instituto Bernabeu we make available to our patients all the technology in our power. That is why we use both the classic techniques and the most innovative studies to be able to give a personalized response to each of our couples.
BIBLIOGRAPHY
- Routine endometrial receptivity array in first embryo transfer cycles does not improve live birth rate. Carrie Riestenberg, M.D., Lindsay Kroener, M.D., Molly Quinn, M.D., Kaycee Ching, B.S., Gayane Ambartsumyan, M.D., Ph.D.
- J Assist Reprod Genet. Evaluation of the endometrial receptivity assay and the preimplantation genetic test for aneuploidy in overcoming recurrent implantation failure. Mauro Cozzolino, Patricia Diaz-Gimeno, Antonio Pellicer, Nicolas Garrido
Azahara Turienzo, biologist at IBBIOTECH, part of the Instituto Bernabeu group.
