Reproductive biology
Discover in depth the biological processes related to fertilization, embryo implantation and all aspects affecting human reproductive biology.

Vaginal probiotics: what they do and how they help to achieve pregnancies
The microbial species in a woman’s vaginal flora play an important role in good health and prevention of infections. Over 50 microbial species have been identified. Personal hygiene and a healthy, balanced diet are key […]

Septate Uterus: what it is, how it is diagnosed, and its treatment
The uterus, fallopian tubes and vagina (or at least part of it) come from embryonic structures called Müllerian ducts. These are two tubular formations which appear on each side of the body, which join at […]

Embryo transfer: How many embryos should be transferred?
In recent years, thanks to long culture and the use of time-lapse incubators, we have been able to preserve embryos in the in vitro fertilisation (IVF) laboratory until day 5-6 of embryo development. This has […]

The assisted reproduction in humans that we are familiar with today would not have been possible without the discoveries made over 70 years ago.
Simulating the conditions in the uterus. IVF laboratory controls
Specific management and quality control systems are key factors in increasing success rates at in vitro fertilisation laboratories (IVF laboratories). Since 2006, all Instituto Bernabeu clinics have adhered to official international ISO 9001 quality management […]
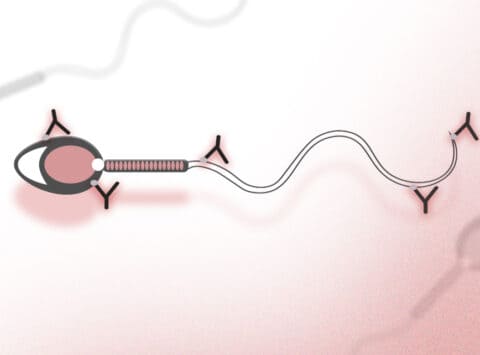
Antisperm antibodies (AAE); What is a myth and what is reality?
Now we are more than used to the word antibodies, and what they are for, which is to protect us against infections, could it be that there were antibodies capable of binding to their own […]

Primary ovarian failure and its diagnosis using mass sequencing techniques
Primary ovarian failure (POF) or early menopause is the loss of ovarian function before the age of 40. As a result of this cessation of ovary function, the woman stops having menstruation and her hormonal […]

From the moment of fertilization, the embryo’s first divisions have been the oocyte responsibility, as the DNA and proteins synthesis took place before fertilization. Therefore, day 3 of embryo culture represents the end of a […]

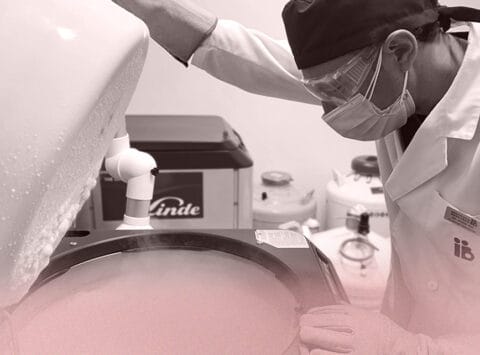
Doubts, questions and answers about egg vitrification
What is the egg vitrification about? Vitrification technique is a relatively new freezing technique based on avoiding the ice crystals formation inside the cells when temperatures below 0 are reached (freezing), therefore, protecting them from […]
What is the spermatogenesis about?
Spermatogenesis is the process of the sperm formation, which are male gametes. It takes place in the testicular seminiferous tubules with an approximate duration of 62 to 75 days in the human species. Sperm formation […]
