Artificial insemination
We explain the treatments and tests involved in this ambulatory assisted reproductive technique, which is often used by women without fertility problems.
The spermatozoa in ejaculate need to have gone through a process known as sperm capacitation in order to obtain the ability to fertilise. This happens naturally in the female reproductive system and techniques in order to […]

Effects of advanced paternal age on fertility
Owing to sociocultural and economic factors, there has been a considerable increase in recent years in the number of men over the age of 35 who wish to have children. As a couple ages, the […]

Embryo transfer on day 4 – why not?
In most laboratories, embryo transfer traditionally takes place on day 2 to 3 of culture, or during blastocyst stage, whilst embryo transfer on day 4 is an alternative that has not commonly been adopted into laboratory practice. When compared with […]
From the very moment when sperm fertilises an ova, a new embryo starts developing and a large number of cell divisions take place. This embryo development is observed in an in vitro fertilisation laboratory up until the […]
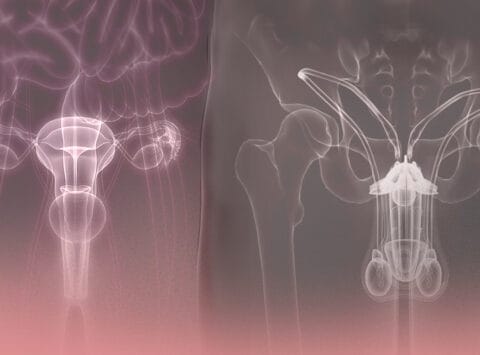
Are sterility and infertility the same? No, they are two completely different concepts. Sterility is the inability to conceive whilst infertility is the inability to complete a full term pregnancy and give birth to a healthy child. […]

What does an embryo biopsy entail?
Pre-implantation genetic diagnosis (PGD) is a technique that provides a ‘genetic understanding’ of the embryo before it is transferred to the uterus. Thanks to this technique, we are able to study the embryo’s chromosomal make-up and […]

Reproduction and genetics guidance
Genetics guidance is the exchange through which an expert in genetics provides patients and their families with information and support on a genetic condition, inheriting that condition, the risk of recurrence and the implications for the individual and his […]

Physiological conditions in embryo culture: reduction of the amount of oxygen in the incubator
Improving embryo culture by mimicking the conditions generated during in vivo culture is a key contributor towards improving success rates in couples who turn to in vitro fertilisation in order to solve their sterility issue. In […]

What became of my embryos? Haven’t I got embryos to freeze?
These are just some of the questions that couples might ask at an important time during their treatment, just before embryo transfer. In all cases of fertility treatment involving the in vitro fertilisation (IVF) laboratory, it is essential that all couples […]

A comparison of the phases in IVF and ICSI treatment
1.- Ovarian stimulation in the patient is carried out by administering doses of hormones that stimulate ovarian function with the aim of achieving sufficient oocytes. The doses of the aforementioned hormones are personalised to each patient […]
