How endometriosis is diagnosed: medical tests and timing
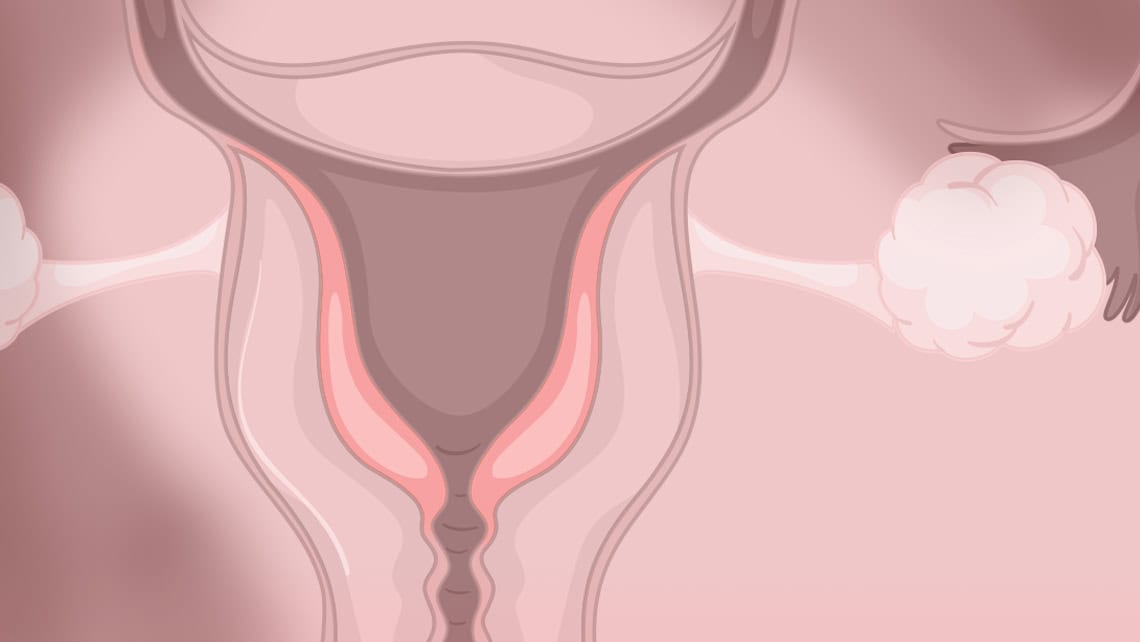
Endometriosis is a chronic benign disease that involves the presence of endometrial tissue outside its usual location. It affects approximately 1 in 10 women and can cause high morbidity, with a significant impact on the quality of life of those who suffer from it.
The diagnosis of endometriosis can not only be complex, but is often delayed, with an estimated average delay of between 8 and 10 years from the onset of symptoms. This is because, to date, there is no single test that can definitively confirm the disease; instead, the diagnosis is based on a combination of symptoms, clinical examination and imaging tests. Surgery, which for years was considered the diagnostic standard, has now been relegated to very specific situations.
Índice
Traditional diagnostic methods
- The first step in diagnosing endometriosis is a detailed medical history, a simple but essential tool. The most common symptoms include severe menstrual pain (dysmenorrhoea), chronic pelvic pain, pain during or after sexual intercourse (dyspareunia), pain when urinating (dysuria) or defecating (dyschezia), most often during menstruation. Cyclical intestinal disturbances such as diarrhoea, constipation or abdominal distension may also occur, as well as sterility or infertility. It is important to note that the intensity of pain does not always correlate with the severity of the disease. On the contrary, some women with mild or even no symptoms may have endometriosis.
- A gynaecological pelvic examination can provide relevant information, especially in cases of deep endometriosis. However, a normal pelvic examination does not rule out the presence of the disease, especially in its early stages or mild forms. Possible findings include pain on uterine mobilisation, the presence of painful nodules in the uterosacral ligaments, palpation of adnexal masses compatible with ovarian endometriomas, or a painful or hardened Douglas pouch.
- There are currently no specific hormone tests or blood markers for the diagnosis of endometriosis. The determination of markers such as CA-125 is controversial. Although this marker may be elevated in some women with endometriosis, it is also elevated in other benign and malignant conditions. For this reason, it is not recommended as an isolated diagnostic test, but rather as a tool for monitoring or assessing response to treatment in previously diagnosed patients.
- For many years, exploratory laparoscopic surgery was the technique of choice for diagnosis, allowing direct visualisation of lesions and histological confirmation by biopsy. Currently, its diagnostic use has decreased significantly, as it is an invasive procedure with risks and possible complications, and current clinical guidelines recommend reserving surgery primarily for therapeutic purposes.
Imaging Diagnostic Methods
- The 2D-3D transvaginal ultrasound performed by professionals with experience in endometriosis is a key diagnostic tool. So-called ultrasound mapping allows for the systematic evaluation of potential disease locations in a non-invasive, accessible manner, and with high precision in expert hands. This technique enables the detection of ovarian endometriomas and deep endometriosis (rectovaginal, intestinal, or bladder), as well as indirect signs such as reduced mobility of pelvic organs or the presence of adhesions.
- Magnetic Resonance Imaging (MRI) is a technique that provides complementary information, although it is not necessary in all cases. It is particularly useful for assessing the extent of deep endometriosis, involvement of the bowel, bladder, or complex anatomical structures, as well as for adequate surgical planning when required.
Recent Methods and Innovations in Diagnosis
- In recent years, non-invasive biomarkers related to endometriosis, such as microRNAs, have been investigated. A microRNA-based saliva test exists, which is a non-invasive test that can help identify women with a high probability of having endometriosis. Although the results are promising, it is currently a complementary tool that does not replace conventional diagnostic tests.
- Menstrual fluid analysis allows for the study of endometrial cells present in menstrual bleeding, as well as certain inflammatory and genetic biomarkers. Although this field of research holds great future potential, it is not yet part of routine clinical practice and is currently in the scientific validation phase.
- New blood biomarkers. Multiple biomarkers, such as proteins, cytokines, and specific genetic profiles, are being researched with the aim of developing reliable diagnostic tests. However, there is currently no validated blood marker for the definitive diagnosis of endometriosis.
How is deep endometriosis diagnosed?
Deep endometriosis is defined as that which infiltrates the peritoneum of pelvic organs by more than 5 mm in depth. Its diagnosis is based on the presence of a characteristic clinical presentation—which may include intestinal or urinary symptoms, or deep dyspareunia—combined with ultrasound performed by expert personnel and, in some cases, supplemented by MRI. Frequently, this type of endometriosis requires a multidisciplinary approach for proper treatment planning.
How is intestinal endometriosis diagnosed?
This type of involvement is usually located in the rectum and sigmoid colon, which are the intestinal structures closest to the internal genital tract. The most common symptoms include pain during defecation, cyclical changes in bowel habits, and, to a lesser extent, rectal bleeding coinciding with menstruation. Diagnosis is primarily performed through transvaginal ultrasound with bowel assessment and MRI. In some cases, a colonoscopy may provide additional information, although it is often normal since lesions are typically located on the outer surface of the intestine.
Frequently Asked Questions
- What are the most common symptoms of endometriosis? The most frequent symptoms are intense menstrual pain, chronic pelvic pain, pain during sexual intercourse, cyclical digestive symptoms, and difficulty achieving pregnancy. Not all patients present the same symptoms or with the same intensity. The absence of symptoms, while making diagnosis less frequent, does not rule out the presence of endometriosis.
- Can I take a test to find out if I have endometriosis? Currently, there is no single, definitive test. Although some non-invasive tests can provide guidance, diagnosis is based on a combination of clinical symptoms and imaging tests.
- Is it the gynecologist who performs the tests? Yes. The gynecologist is the specialist who coordinates the diagnostic process and requests the necessary tests, collaborating with other specialists when required.
- Are the diagnostic tests for endometriosis very invasive? Most current diagnostic tests are non-invasive. Surgery is reserved for specific cases and, generally, for therapeutic purposes.
Dr. Silvia Gorgan, Gynecologist at Instituto Bernabeu Alicante.
