Absent uterus or Mayer-Rokitansky-Küster-Hauser syndrome: what can I do?
Mayer-Rokitansky-Küster-Hauser syndrome – or simply MRKH syndrome – is a congenital disorder (birth defect), the main characteristic of which is that the women who suffer from it do not have a uterus.
The cause of this infrequent condition (1 in 5,000 female births) is an abnormality during development of the internal genitalia during the embryo/foetus stage. As well as an absent uterus, affected women also tend to have an absent vagina (this can be either partial or complete).
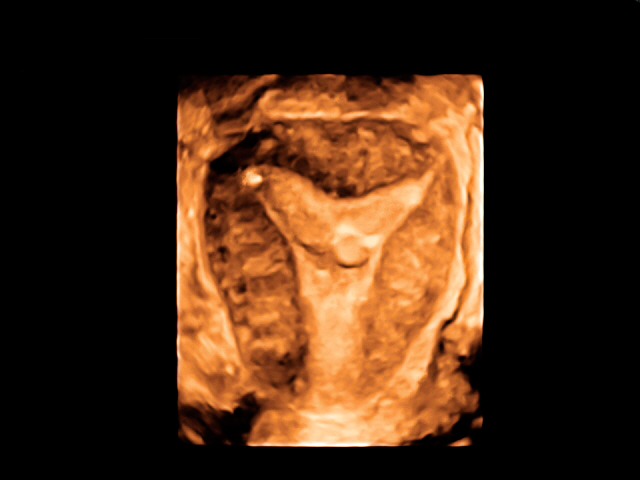
From a fertility point of view, these patients clearly cannot gestate precisely because of this absence of a uterus or womb. However, it is important to highlight that ovary development is not affected by the syndrome. In other words, female hormones are produced as normal during puberty and, therefore, the young woman develops sexual characteristics as normal (breasts and pubic hair, for example), except for periods. Amenorrhea (an absence of menstrual periods) is, therefore, usually the initial symptom that leads to a diagnosis which is later confirmed using an ultrasound scan or magnetic resonance scan.
From the point of view of assisted reproduction techniques, and since the woman’s ovaries are intact (making it possible to retrieve ova for in vitro fertilisation), the work focusses on ‘solving’ the issue of the absent uterus. The technique that is most commonly used in these cases is called surrogacy, which entails transfer of embryos to another woman who has a complete uterus and who can gestate. This technique is used in some European countries but legal regulations mean that it cannot be used in Spain.
More recently, so-called uterus transplantation has been described. It is a technique that consists of transplanting the uterus from another woman to a patient who has Mayer-Rokitansky-Küster-Hauser syndrome so that she can gestate. Following a successful birth after use of this technique in Sweden, a second successful case was recorded in the United States of America. However, the technique is still incredibly complicated and involves considerable surgical interventions.
Last of all, whilst modern 3D structure printing technology means that it is possible to design organs and tissues (including the uterus and endometrial cells) that could accept embryos, experiments such as these could imply insurmountable ethical challenges in terms of making them a clinical reality. This is certainly the situation for the near future.
Dr Juan Carlos Castillo, a gynaecologist at Instituto Bernabeu.
