Types of endometrial receptivity test. Pros and cons
Embryo implantation in the endometrium is still considered a critical step in achieving pregnancy, and occurs in a brief period of time when the endometrium expresses specific molecules that allow the embryo to nestle in, known as the ‘implantation window’.
Embryo implantation failure is a phenomenon that has been extensively studied in reproductive medicine, particularly at Instituto Bernabeu, where we carry out various R&D&I programmes within our Implantation Failure Unit.
The limitation of classic morphological and ultrasound markers in accurately identifying the ideal moment for implantation has driven the development of molecular tests (transcriptome, microRNA and other panels) that attempt to define this optimal moment more precisely.
However, the evidence accumulated in recent years calls into question their usefulness and clearly restricts their indications.
Índice
What is the endometrial receptivity?
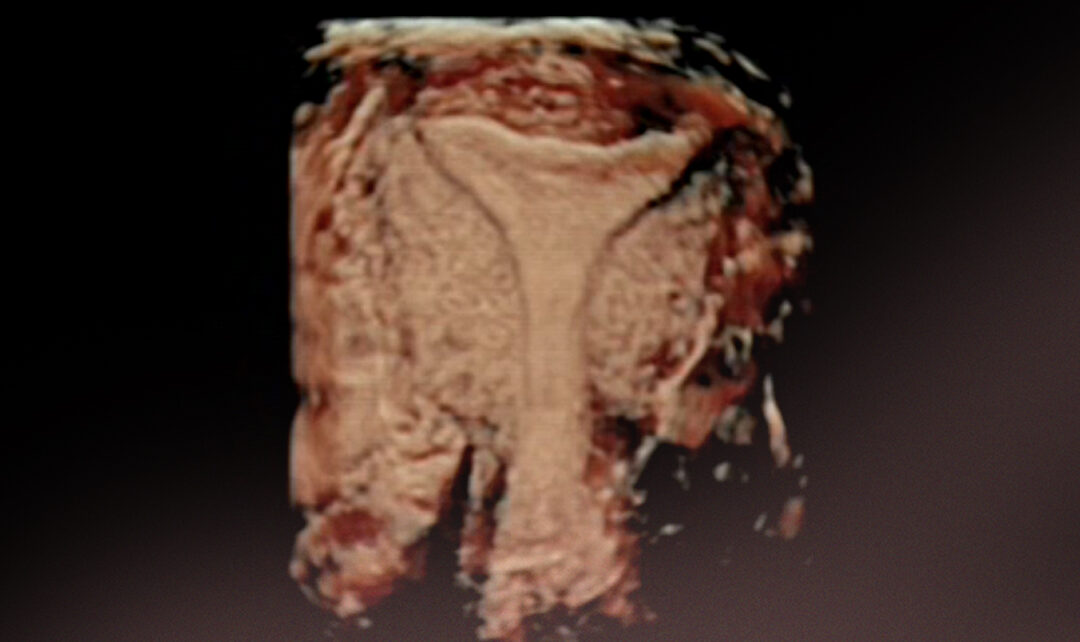
The endometrium is the tissue that lines the uterine cavity. For implantation to occur, the endometrium must be prepared to ‘accept and welcome’ the embryo.
This state of the endometrium is called endometrial receptivity and has been found to occur only at a specific time, around days 20-21 of a natural menstrual cycle or around 5 days after starting progesterone in substituted cycles, constituting the implantation window.
A characteristic gene expression profile has been described during this window, and it is known that some women with recurrent miscarriages or implantation failures have altered expression of these markers.
What kind of tools we have to study endometrial receptivity?
Histological analysis of endometrial biopsy
Since Noyes established different patterns in the endometrium cellular structure throughout the menstrual cycle in the 1950s, endometrial biopsy has been the technique of choice for this purpose.
The problems with biopsy are that it is an invasive procedure that can cause discomfort, bleeding or even infection, and that its ability to accurately determine the implantation window is limited.
Ultrasound techniques
EnUsually, endometrial visualisation has been performed by ultrasound. There are several parameters to consider when determining endometrial receptivity:
- Endometrial thickness
- Ultrasound pattern
- Endometrial volume
- Uterine contractility
Although these are useful tools, they alone cannot predict endometrial receptivity, and there are many patients who continue to experience implantation failure even with good ultrasound images.
Endometrial genetics tests
These tests attempt to determine the implantation window more accurately based on gene or microRNA expression. They are grouped into two main families:
1) Transcriptomics-based tests (ERA, ER Map, etc.)
2) MicroRNA-based tests (MIRA and others in development)
Endometrial receptivity test based on the transcriptome
By studying the transcriptome, we can determine more accurately which genes are active or inactive in a given cell type or tissue at a specific time.
ERA (Endometrial Receptivity Array) tests and derivatives use this transcriptomic technology to classify the endometrium as pre-receptive, receptive, or post-receptive and propose a ‘personalised implantation window’.
These tests are more accurate than classical histology and can identify differences in the implantation window in patients with recurrent implantation failure (RIF).
Endometrial receptivity test based on microRNA expression
MicroRNAs are very small RNA molecules that regulate gene expression and are closely involved in the embryo implantation process.
Recent studies reveal that miRNAs not only act inside cells, but can also be released into the extracellular environment and serve as non-invasive biomarkers for assessing endometrial receptivity.
Currently, these types of tests are still in the development and validation phase. There are no robust clinical trials demonstrating that they improve live birth rates compared to standard practices. In fact, their use is restricted and they are still considered a research tool.
For or against endometrial genetics tests for endometrial receptivity?
Currently, thanks to recent advances, we can take a more informed stance when it comes to positioning ourselves for or against these tests:
– They can be beneficial when performed on very specific groups of patients. Those with recurrent implantation failure, with good quality embryos and after ruling out other causes (uterine, thrombophilia, serious male factors, etc.).
– However, they will not be very helpful if we perform them routinely on all patients with no history of implantation failure.
Therefore, today the most widely accepted strategy is to integrate them as one more tool, not as a unique one, within a comprehensive and personalised approach that includes classic uterine assessment, embryo quality, endocrine, immunological and genetic factors.
At Instituto Bernabeu, we make all the technology at our disposal available to our patients. That is why we use both classic techniques and the most innovative studies in order to provide a personalised response to each of our patients.
Azahara Turienzo, biologist at IBBIOTECH, part of the Instituto Bernabeu group.
