Polycystic Ovary Syndrome
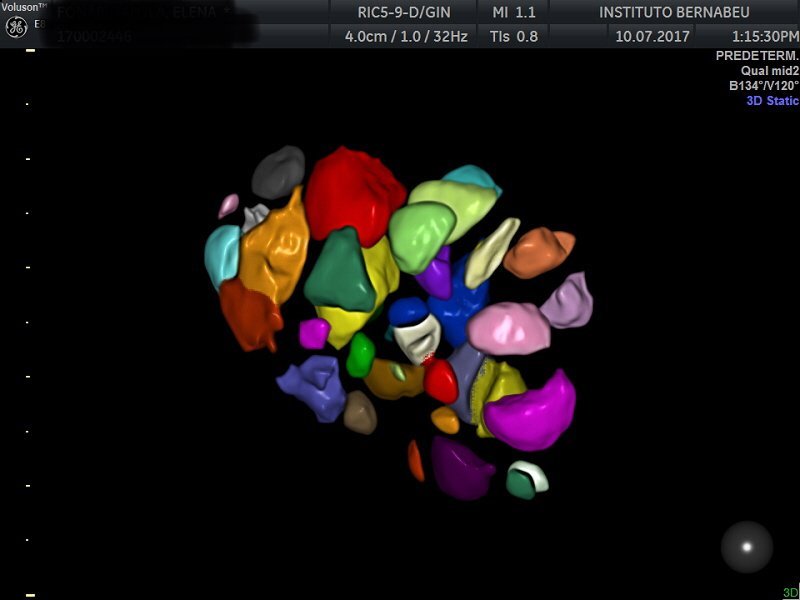
The term polycystic ovary syndrome is used to define an ultrasound diagnosis characterised by the presence of 12 or more follicles in each ovary (between 2 and 9 mm in diameter) and/or an incremented ovary volume (>10 ml). Findings such as these in ultrasounds in a single ovary are sufficient in order to be able to give a diagnosis. However, since taking oral contraceptives can change ovary morphology, this diagnostic criteria does not apply to women who take oral contraceptives.
From a practical point of view, when assisted reproduction technology (ART) is being used, detection of polycystic ovaries in isolation is useful for predicting the ovary’s response to stimulation using drugs and the risk of ovarian hyperstimulation syndrome.
It should be differentiated from POLYCYSTIC OVARY SYNDROME (PCOS) which is an ovarian dysfunction pathology that can have an impact on fertility and can involve an increased risk of metabolic diseases later on in life.
PCOS is a syndrome and, as such, just a single criterion is insufficient for reaching a diagnosis. In 2006, the American Society of Reproductive Medicine and the European Society of Human Reproduction and Embryology met in the Dutch city of Rotterdam in order to come to a consensus and define this complex pathology. Since then, PCOS has been defined as the presence of at least two of three possible criteria in the patient:
- Oligoovulation and/or anovulation
- Clinical or biological signs of androgen excess
- Polycystic ovaries
Oligoovulation is the presence of irregular periods with menstrual cycles in excess of 35 days, or fewer than 8 periods in a year. Anovulation is an absence of ovulation that is clinically present as irregular, frequently unpredictable cycles, occasional presence of amenorrhea (absence of periods) and, in other cases, abundant periods (dysfunctional uterine haemorrhage).
Hyperandrogenism is an androgen (male hormone) excess in the body. This phenomenon can be clinically diagnosed through hirsutism (hair in places on the body that is unusual in women. For example, facial hair or chest hair), acne and alopecia. A diagnosis may also be reached biochemically by measuring levels of testosterone in the body.
PCOS mainly affects fertility by interfering with ovulation and altering menstrual cycles so that ovulation ends up being unpredictable. Therefore, the first means of treatment is the use of drugs such as clomiphene citrate to induce ovulation. If this first course of treatment is not successful, the next step is artificial insemination or in vitro fertilisation.
Some patients can benefit from the ovarian puncture-aspiration of visible antral follicles technique. It is performed with the use of an ultrasound scan in order to try and achieve normal ovarian function before embarking on more complex techniques. Patients must not have any other causes of sterility. The procedure is performed with the patient under sedation and no over-night hospitalisation is required. The patient has ultrasound scans and blood tests following the intervention in order to detect ovulation. This enables us to schedule sexual intercourse if necessary or even attempt in vitro fertilisation treatment if the patient does not ovulate and/or achieve a pregnancy. The success rates for this technique are similar to those achieved with surgical drilling (performed using a laparoscopy). However, it has fewer complications.
Last of all, it should be pointed out that, due to the metabolic nature of this pathology, women with PCOS are at an increased risk (3 to 7 times greater) of having type 2 diabetes, heart diseases and dyslipidaemia. An increased risk of endometrial cancer has also been noted due to chronic anovulation that exposes the endometrium to a prolonged presence of oestrogen.
It is clear that dealing with patients who have PCOS does not consist exclusively of treating reproduction issues. It also requires a multidisciplinary approach by gynaecologists, endocrinologists and nutritionists in order to minimise the risk of illnesses later on in life.
Dr Juan Carlos Castillo, gynaecologist at Instituto Bernabeu
