Vasectomies: the male contraceptive
Índice
- 1 What is a vasectomy?
- 2 How is vasectomy done?
- 3 Is vasectomy effective?
- 4 Is vasectomy safe?
- 5 Can vasectomy be reverted? What is the vasovasostomy?
- 6 What are the vasectomy risks?
- 7 Is vasectomy painful?
- 8 What are the differences between scalpel and no-scalpel incision vasectomy?
- 9 What are the vasectomy’s side effects?
- 10 How long will take to recover from vasectomy?
- 11 When sexual relations can be retaken after vasectomy?
- 12 What are the vasectomy benefits?
What is a vasectomy?
Vasectomy is a minor surgery procedure to prevent having children permanently. Is the most effective male sterilization technique in comparison with all others and is done with the final idea of having no more children.
How is vasectomy done?
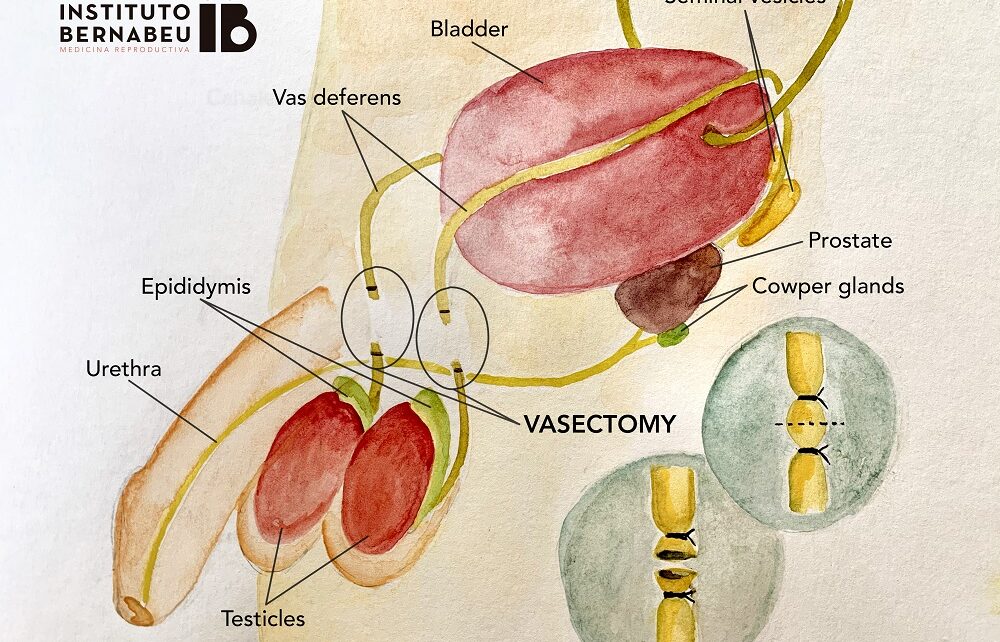
Is a precise and simple surgical intervention with local anaesthesia. Consist of the cut and obstruction of both testicles’ vas deferens, which takes the sperm to be ejaculated. The vas deferens is cut off, bonded and interjected in different layers for a definitive interruption. As a consequence, the sperm will end up without spermatozoon and will prevent having children in a natural way.
On most cases, we perform this intervention as outpatient and with local anaesthesia. Is performed in 20-30 minutes and the recovery is usually quick, easy to cure and stiches fall off by themselves.
Is vasectomy effective?
Vasectomy is the male’s most effective contraception technique to avoid unwanted pregnancies. Is effective once is confirmed the absence of sperm in the sperm analysis; this happens around the 4th and 6th month after the intervention. A confirmation analysis must be done to make sure there are no spermatozoon in sperm.
Is vasectomy safe?
Is a minor procedure done by experts, under local anaesthesia and low risk. Once the sperm analysis is checked, is the most effective and final sterilization technique.
Can vasectomy be reverted? What is the vasovasostomy?
Although vasectomy is done with a definitive idea, it might not be so definitive. There are two alternatives to become fertile again:
- To revert a vasectomy or reconduct it we may undergo an intervention called vasovasostomy. Is a microsurgery whereby the ducts are rechannelled to permeabilise it allowing natural conception. This technique achieves higher success rates if done within 8 years since the vasectomy was done. After this period, results decreases. In the first case results might be between 80 – 90 per cent. We have a vast experience, as we know the results success depends mostly on the precise surgical technique and time since vasectomy was performed.
We can retrieve the sperm directly from his testicles through fine needle puncture and aspiration (FNPA), and use the collected sperm for the assisted reproduction treatment.
What are the vasectomy risks?
Vasectomy risks are low. The same as any other procedure with local anaesthesia. If any complication, these are usually minimal and not serious. Only 5% may present scrotal hematoma, scrotal pain which is usually controlled and easy to treat. We must not forget a less frequent complication, the vasectomy failure, whereby there’re still spermatozoon present in the sperm after a year from the surgery. This happens in one of 10.000 men with vasectomy, this makes a second intervention recommendable.
Is vasectomy painful?
Keeping in mind the personal pain sensibilization, vasectomy is not usually painful and is done under local anaesthesia. In some cases, it can also be done under sedation. Obviously, there’s no need to suffer pain to undergo these types of techniques.
What are the differences between scalpel and no-scalpel incision vasectomy?
Marketing aside, there aren’t relevant differences between no-scalpel vasectomy, incisional vasectomy and bilateral vasectomy (the most used). This is because the vasa deferentia must be tied at each side and the pain comes mostly from interna tissues as the cuts are minuscule. To exteriorize the deferens is not an advantage, is as painful and offers same effectiveness. Same thing happens when there’s just one incision in the middle to gain entry to both conducts.
We offer all these techniques and let the patient to choose advising there’re no significant differences in pain and effectiveness between them.
What are the vasectomy’s side effects?
There is some concern in men about the possible loss of masculinity when undergoing a vasectomy, mistakenly thinking that the intervention involves castration. However, it is clearly demonstrated that vasectomy does not produce any alteration in the man’s sexual potency of, neither in orgasm, nor in sexual desire. These phenomena remain the same as before the intervention.
Among the vasectomy’s side and harmful effects, there are many myths and false beliefs, thinking about the effect of this surgery on men’s health. An attempt has been made to find a direct relationship between vasectomy and cardiovascular disease, diabetes, testicular cancer and prostate cancer. However, many scientific studies have shown that there is no relationship between vasectomy and these diseases. Other possible effects are the psychological disorders derived from the intervention (anxiety, depression and regret for having the vasectomy done). To clearly inform about the intervention would avoid these effects.
How long will take to recover from vasectomy?
Recovery from vasectomy is quite quick and allows carry out activities from the first day after its completion. Certain jobs involving physical exercise or sports require a certain level of rest, as well as avoiding swimming pools, sea baths, as in any surgical intervention, for approximately two weeks or when the wounds are well healed.
When sexual relations can be retaken after vasectomy?
Sexual abstinence is medically advised for a few days after vasectomy. It is advisable not to have sexual intercourse for at least two weeks, until the vasectomy wounds are healed, mainly because they could become infected and also because testicular discomfort can also be experienced.
What are the vasectomy benefits?
Vasectomy advantages are beyond question. Establishes definitive infertility so as not to have more children without the need to use contraception methods. Benefits stars as soon as the sperm analysis confirms there are no more spermatozoon.
Dr Luís Prieto, director of urology at the Instituto Bernabeu
IT MAY ALSO BE OF INTEREST TO YOU
- Andrology at instituto Bernabeu
- How to be a parent after vasectomy?
