Semen quality parameters according to the World Health Organisation (WHO)
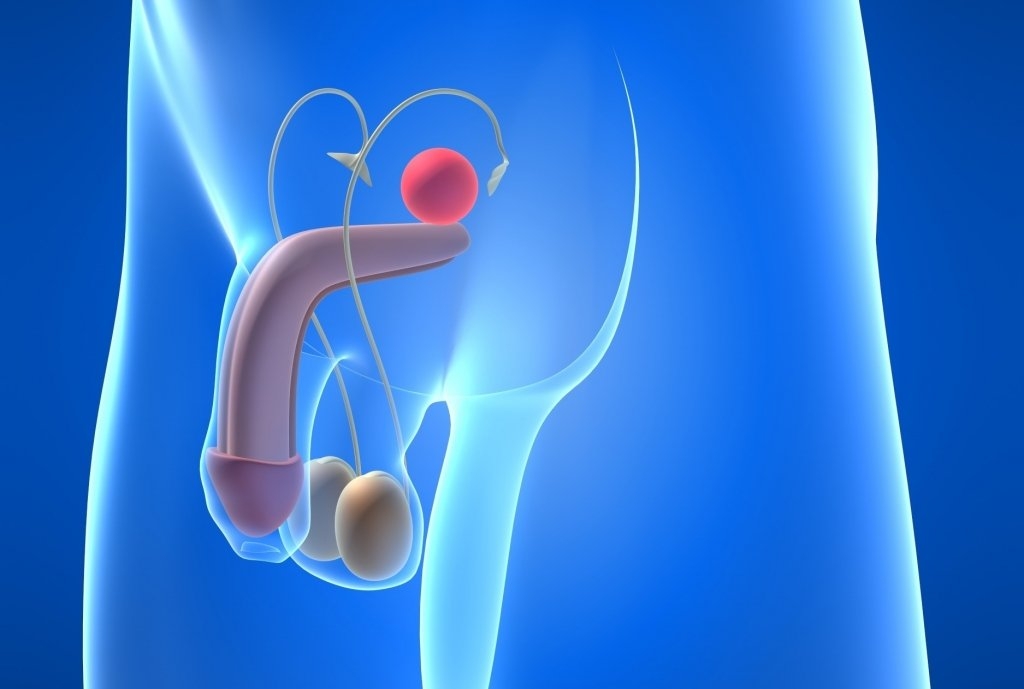
The spermiogram is a basic tool that provides us with some of the best information to assess male fertility. It is also very useful in order to formulate a personalized treatment plan for the couple.
Conventional analysis of the semen quality, or semen analysis, is the basic routine tool that provides information about the male reproductive potential, and is very useful when indicating personalized treatments for the couple. The need to increasingly define the seminal characteristics of both fertile and infertile males has led the World Health Organization (WHO) to publish successive editions of the “Manual for the examination and processing of human semen”, the current edition being that of 2010 (5th edition). This manual serves as a guide in andrology laboratories, standardising the method of assessing semen quality.
Índice
SEMEN PARAMETERS (WHO 2010)
There are many parameters to take into account in a semen analysis, which can be divided into those that can be evaluated with the naked eye (macroscopic examination) and those that cannot be evaluated with the naked eye (microscopic examination). Below, we show the requirements that a semen sample must meet in order to be catalogued as normal (Normozoospermia):
MACROSCOPICS FACTORS
Liquefaction
After ejaculation, semen is in a coagulated state and needs to be liquefied in order to be studied. A semen sample liquefies completely in approximately 15-20 minutes at room temperature. If complete liquefaction does not occur within 60 minutes, the semen sample can be subjected to mechanical liquefaction in order to analyse the rest of the parameters.
Viscosity
It refers to the fluidity of the entire sample, which can be normal or high. The methods to reduce viscosity are the same as those for liquefaction. If the sample presents high viscosity levels it may be due to a prostatic dysfunction.
Volume
The normal volume of an ejaculate, after 3 to 5 days of sexual abstinence, is in the range of 1.5 to 6 mL. A lower volume is called Hypospermia, while a higher volume is called Hyperspermia. The absence of semen with ejaculation is known as Aspermia.
Colour
The usual colour of semen is opalescent white, slightly yellowish. In cases where the colour is altered, it is advisable to study the possible causes. An example of alteration would be the presence of red blood cells in the semen sample (Hematospermia).
pH
This value must be over 7.1. Lower values and a low sperm concentration could indicate efferent vessel dysgenesis, i.e. a blockage of the ejaculatory ducts.
Concentration
The normal value is 15 million spermatozoa per millilitre of ejaculated volume or 39 million in the entire sample. If these values are not reached we would be talking of Oligozoospermia and, in the most severe cases, of Cryptozoospermia (<100,000 spermatozoa/mL).
Motility
The percentage of motile and progressive (spermatozoa moving actively) sperm are assessed. Progressively motile spermatozoa must exceed 32%; otherwise, it is called Asthenozoospermia.
Vitality
The percentage of live spermatozoa must exceed 58%. If it were lower, we would be talking about necrozoospermia.
Leukocytes
If the concentration of leukocytes is greater than 1 million per mL of sample (leukospermia) it may indicate a genitourinary infection.
Morphology
In a normal semen analysis, there should be equal to or more than 4% of normal spermatozoa. If the value is below this range, this is known as Teratozoospermia.
Anti-sperm antibodies or MAR test
It indicates the amount of spermatozoa attached to other cells or particles. When more than 50% of spermatozoa are bound to, it may reflect an immune problem.
COMPLEMENTARY EVALUATIONS
Nevertheless, there are other additional tools that can improve the information obtained through the conventional semen analysis. We can know, through different molecular techniques, the functional competence and the genetic characteristics of the spermatozoa population, such as the evaluation of sperm DNA fragmentation (TUNEL) and fluorescence in situ hybridization (FISH).
Bibliographical references
- World Health Organization. “WHO Laboratory Manual for the examination and processing of human semen” Cambridge: Cambridge University. fifth Edition (2010).
