Endometrial polyps: what are they, how are they formed and what are the symptoms and treatment?
Índice
- 1 What are endometrial or uterine polyps?
- 2 Types of endometrial or uterine polyps
- 3 What causes endometrial or uterine polyps?
- 4 Endometrial or uterine polyp symptoms and/or complications
- 5 Endometrial or uterine polyp diagnosis
- 6 Treatment of endometrial or uterine polyps
- 7 Endometrial polyps and pregnancy
- 8 Can endometrial or uterine polyps be avoided?
What are endometrial or uterine polyps?
Endometrial polyps are cell formations that project from the endometrial cavity.
They are a common gynaecological pathology experienced by 20% of women. They appear most commonly in women aged between 40 and 65. However, women of all ages can have them.
They contain endometrial glands, stroma and blood vessels. They attach to the uterine wall across a more or less significant surface area.
Types of endometrial or uterine polyps
Polyps can be categorised based on:
- Number (single or multiple)
- Size
- Position in the uterus (fundal, cornual, lateral, isthmic and so on)
- The implantation base (pedunculated, sessile and so on)
- Histologic characteristics (functional, hyperplastic or atrophic)
Most polyps are benign. However, between 0.5 and 1% of them can lead to cancer. Transformation of this kind is linked to predisposition factors including the menopause, obesity, oestrogen therapy, patients who have taken tamoxigen and links to colon cancer.
What causes endometrial or uterine polyps?
Oestrogen levels – both excess levels and hormone imbalances – play a significant role in the formation of polyps. Certain factors can predispose women to uterine polyps. These include:
- Having undergone hormone therapy with oestrogen with no compensation for this using progesterone
- Taking tamoxifen
- Advanced patient age
- Obesity
- Hypertension
- A medical history of colon cancer, etc.
Endometrial or uterine polyp symptoms and/or complications
In most cases, there are no associated symptoms and polyps are discovered during ultrasound scans in routine gynaecological check-ups, during treatment to freeze ova, sterility treatment and so on.
Women who do have symptoms most commonly have irregular uterine bleeding. This tends to be light.
Women can also experience changes in their menstrual bleed, increased menstruation, postmenopausal bleeding, bleeding during sexual intercourse and so on.
Large polyps can cause small contractions in the uterus that cause abdominal pain.
Sometimes, particularly if the polyps are larger than one centimetre, they can be associated with infertility or recurrent pregnancy loss since they complicate correct embryo implantation. When the reason for patients’ infertility is unknown, determining if a woman has endometrial polyps is recommendable.
Endometrial or uterine polyp diagnosis

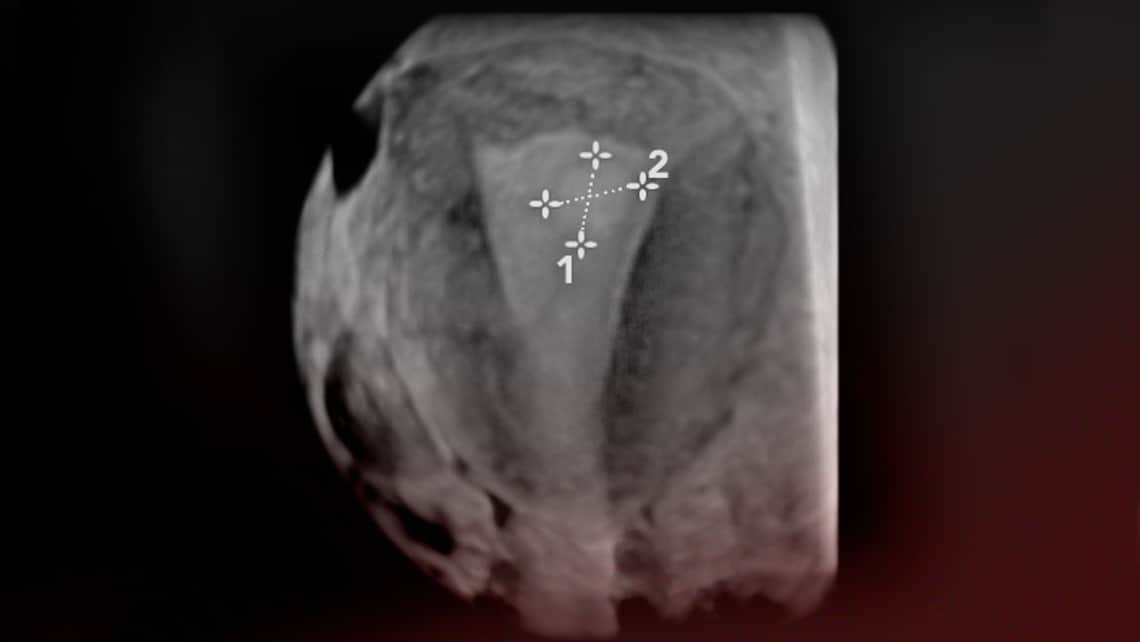
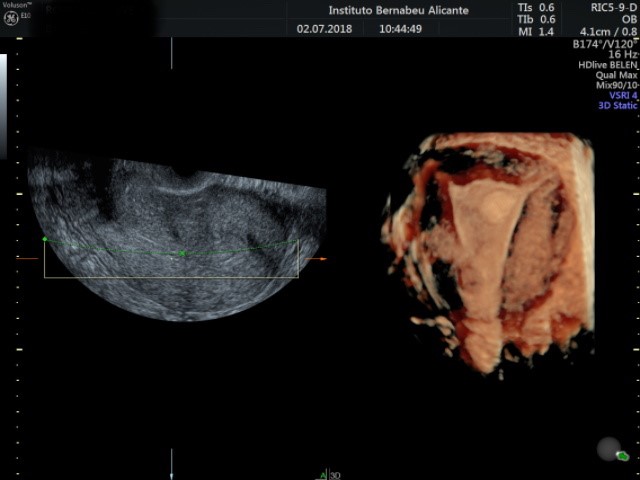
A transvaginal ultrasound is the method of choice in order to reach a confirmed diagnosis. In addition, a 3D ultrasound can provide an accurate diagnosis. Sonohysterography procedures can sometimes prove helpful. This consists of introducing saline solution into the endometrial cavity so that the area surrounding the polyp can be observed with an ultrasound.
A hysteroscopy can be performed to confirm the diagnosis. This entails inserting a camera into the uterus so that the uterine cavity can be observed directly. In addition to confirming what was observed in the ultrasound, a hysteroscopy facilitates histopathological analysis when there is a suspicion that polyps are malign. It also makes removing them possible. A hysteroscopy test can be performed in day clinics. Sometimes, the patient needs to be sedated but recovery is swift.
Treatment of endometrial or uterine polyps
A polypectomy is advised when polyps are in excess of 1cm and whenever the patient has any of the symptoms associated with endometrial polyps. Likewise, when patients are undergoing an analysis of sterility with an unknown cause or recurrent pregnancy loss, removal of polyps is recommended, irrespective of their size.
If polyps are small, they can be removed using a diagnostic hysteroscopy with instrumentation that is smaller in diameter. On occasions, this can be performed without the need to sedate the patient. When polyps are larger, patients need to be sedated and surgical hysteroscopy is required (larger diameter with the option of coagulation at the polyp implantation base).
Endometrial polyps and pregnancy
Polyps can have an impact on fertility for a range of different reasons:
- For example, size, which stops the embryo from implanting or encourages recurrent pregnancy loss.
- Location is also another factor since it obstructs the tubes in the uterus.
When patients suffer from implantation failure and recurrent pregnancy loss, we recommend carrying out a hysteroscopy in order to assess the uterine cavity and rule out any pathologies in the endometrium, and performing a polypectomy if there are any endometrial polyps.
Can endometrial or uterine polyps be avoided?
The best way of preventing endometrial polyps is a regular, annual gynaecological check-up so that an early diagnosis can be reached.
Of course, patients whose infertility has an unknown cause can put themselves in the hands of experts in the field. Specialists can perform a comprehensive and exhaustive assessment of the situation.
Dr Cristina Gavilán, a gynaecologist at Instituto Bernabeu.
